- Tooth decay occurs when plaque formation produces acids that attack the hard tissues of the teeth. The lack of proper oral hygiene and a diet high in simple sugars can accelerate this process.
- Root decay is particularly common in patients with receding gums and in the elderly.
- The type of treatment a dentist will use depends on the severity of the tooth decay. Fluoridation, fillings or crowns, and abscess intervention are just some of the possible treatments.
Need urgent dental care? Use Authority Dental to quickly connect with emergency dental clinics in your city.
Have you noticed the decay on your teeth? Here's everything you need to know.
What causes tooth decay?

Picture by Authority Dental under CC 2.0 license
The condition is more of a process. To put it simply, food debris that is left behind turns into acids that attack the teeth. This happens when patients neglect to conduct proper oral hygiene that includes brushing, flossing, and having professional cleanings in an oral environment favorable to decay.
Risk factors of dental caries include:
a diet rich in carbohydrates and acids,
conditions that inhibit the production of saliva,
certain medications, and
some oral conditions.
Disorders such as diabetes mellitus and Sjögren’s syndrome may lead to decreased saliva flow. This substance is helpful in thinning down and washing away bacteria between brushing sessions. Some medications, especially antihistamines and antidepressants may also make this worse.
Other issues, like receding gums and periodontitis, may likewise increase risk of decay.
Types of dental caries
Dental caries are categorized according to their location.
Pit and fissure and occlusal caries
Pit and fissure and occlusal caries are generally the same. The latter refers to the biting surface of the posterior teeth. Pits and fissures are found on this surface, with some extension to the cheek and tongue sides.
Decay on smooth surfaces of dentition is usually easy to spot and quick to diagnose. Molar teeth are likely to be affected, as they are in the back and harder to brush properly. This is why flossing is vital.
A good preventative method is a dental sealant. A thin coating is placed in those nooks and crannies to avoid having food getting stuck there. The layer bonds to the teeth.
Root caries
If decay happens below the gumline it is considered root decay. This is a dangerous type of cavity, as it happens on the cementum. This is softer, thinner, and more vulnerable than enamel.
Decay can reach the pulp sooner than if the cavity had started on enamel. Root caries are common among patients with receding gums and in the elderly. They develop twice as fast as cavities in other areas of the tooth.
Tooth decay stages
Knowing how tooth decay develops can help you adjust home remedies and prepare for your dental visit.
Initial demineralization
The first stage of tooth decay is demineralization of the enamel. This is the outer shell of the tooth, a very hard substance made up of different minerals. Acids produced by bacteria dissolve the structure and this shows up as chalky white spots on the teeth.
Enamel decay
If the acids and bacteria are not removed, and the teeth are not remineralized, decay of the enamel begins. This looks like darker, brown spots. These can quickly turn into lesions requiring a filling.
Up until this point, the process is reversible. If the patient neglects to address the issue, however, tooth structure can be lost. And it cannot be recovered without dentist intervention. The affected area may turn soft to the touch.
Dentin decay
Dentin is right under the enamel and it is much softer. Decay happens a lot faster at this stage. What’s more, dentin has tubes that connect to tooth nerves.
Patients may experience sensitivity, especially to hot, cold, and sweet foods and drinks. Bad breath and a foul taste in the mouth is also common.
Pulp damage and death
The innermost layer of the tooth has nerves and blood vessels. If this tissue becomes irritated, it starts to swell. Cracks and fractures may appear, as the tooth structure becomes undermined. This is also often painful.
If it comes to the death of the pulp tissue, the tooth will stop being sensitive to any stimuli, but may be tender when pressed. Pain to chewing may develop, as well as swelling in the gums and even on the face.
Can you reverse tooth decay?

Picture by Authority Dental under CC 2.0 license
If the dentin has not yet come to any damage, decay can be reversed. There are some home remedies you can try, but a dental visit with a professional is always recommended. You may not be able to assess or diagnose the issue yourself.
While waiting for your appointment, you can:
incorporate fluoride and vitamin D in your diet,
consider buying toothpaste with fluoride,
chew sugar-free gum, and
try oil-pulling.
Any products with fluoride will help remineralize your teeth. It is present in some tap water across the US. Further demineralization can be prevented by chewing sugar-free gum. Most brands use xylitol, which can stimulate the production of saliva, neutralize the mouth’s pH, and help kill some bacteria.
Vitamin D is an important component of making your teeth healthy. You can find it in foods like milk and yogurt as well as in your garden.
Sesame or coconut oil can be used to clean your mouth. Swish some around in your mouth for about 20 minutes and spit it out. It may be a good idea to brush your teeth afterwards anyway. This is a home remedy, not a professional recommendation.
Tooth decay treatment
The type of treatment your dentist will go with depends on how severe your tooth decay is. He or she will begin with an exam to diagnose the problem and stage of the caries. Talk about any pain or sensitivity you have experienced. There might also be some X-rays and a probing session.
Fluoridation
If your tooth decay has not gotten past chalky white spots, fluoridation may be enough. Fluoride varnish will be applied to the affected teeth. This is totally non-invasive and you will not need any anesthesia.
The dentist may also apply fissure sealants to your molar teeth to prevent decay in the future. You might receive a prescription to use fluoridated toothpaste and mouthwash at home.
Fillings or crowns

Picture by Authority Dental under CC 2.0 license
If the tooth structure has been lost, you will need a filling. The damaged area will be drilled away under a local anesthetic to numb any discomfort. Then, either composite resin or amalgam will be used to fill the hole and build up the tooth.
When decay has eaten away at a large part of the tooth, you may need a crown. Some healthy structures may also have to be removed to accommodate it. A porcelain “cap” will restore your smile’s appearance.
Abscess intervention
If an abscess has formed, it will need to be professionally removed. Do not attempt to burst it yourself, as the infection might travel towards the inside of your body.
The dentist will make a cut and release the liquid. This relieves pain significantly. The area will then be cleaned with saline solution. A root canal procedure may be necessary. In cases where the patient’s immune system is weakened or if the infection has spread considerably, an antibiotics treatment is prescribed.
Root canal treatment
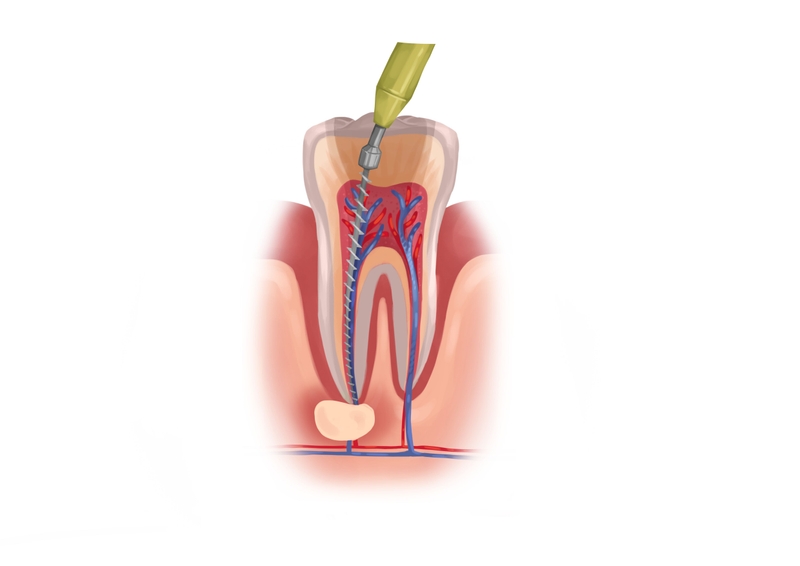
Picture by Authority Dental under CC 2.0 license
If the dental pulp was infected, you will likely need endodontic treatment. This means drilling a hole through the top of your tooth and removing all damaged matter from the inside. It may take several visits and you might have to take antibiotics. The root canal treatment will often end with a large filling or crown.
Extraction
Sometimes the damage is so large, the tooth has to be removed to prevent further infection of other dentition and the rest of your body. Your dentist will discuss restoration options such as dental bridges and implants with you. Not replacing a pulled tooth could cause your other dentition to shift and your face to appear to sag due to a loss of support.
FAQ
FAQ
How does plaque lead to tooth decay?
What are the most common tooth decay symptoms?
Can you remove tooth decay yourself?
How can you stop tooth decay?
If you notice white spots on your teeth, make sure you drink fluoridated water and switch to a toothpaste that contains this mineral. Avoid acidic and sugary beverages. Even sugar-free ones with acids in them will erode enamel.
Make an appointment with your dentist to check out whether everything is okay. Drilling and filling may be unnecessary if you act quickly.
What if you don’t treat dental cavities?
Such neglect can cause an abscess to form. This happens at the stage when the decay attacks the pulp. The gums become inflamed and a pus pocket forms near the tooth.
This is urgent. The tooth may be lost, and the disease can spread via the bloodstream to the rest of the body. It puts the patients at risk of sepsis.
Can a badly decayed tooth be saved?
How to prevent tooth decay?
Prevention begins at home. Brush after every meal and use floss and mouthwash once a day. Try not to eat sweet snacks full of carbohydrates, especially when you’re out and have no way of cleaning your teeth. Any snacking should be avoided, as it raises your mouth’s pH for about 30 minutes.
Make sure to stay up-to-date with regular dental check-ups and cleanings. Incorporate fluoride into your diet and homecare routine to keep your teeth mineralized.
References
- The relationship between oral health and diabetes mellitus
- Sjögren Disease
- Salivary Secretory Disorders, Inducing Drugs, and Clinical Management
- Pit and fissure sealants for preventing dental decay in permanent teeth
- Interventions for managing root caries
- Demineralization–remineralization dynamics in teeth and bone
- Community Water Fluoridation
Peter March, DDS
Sealants are typically covered by insurance for children. As an adult, they are still very beneficial even if insurance states that they are not a covered benefit.