- Root decay occurs when bacteria multiply and produce acid that breaks down the cementum layer of the tooth. Poor oral hygiene is the main cause of tooth decay.
- Symptoms of root decay include toothache, difficulty in chewing, sensitivity to hot and cold temperatures, and discoloration of the teeth. Progressed decay causes abscesses, redness, pus and swelling of the gums, and loose, broken, or cracked teeth.
- If caught early, it can be treated without invasive measures.
Save your teeth from root decay. Use Authority Dental to book a urgent dental appointment and get a same-day treatment.
Have you noticed caries on the root surface of your tooth? Here's everything you need to know.
What is root decay?

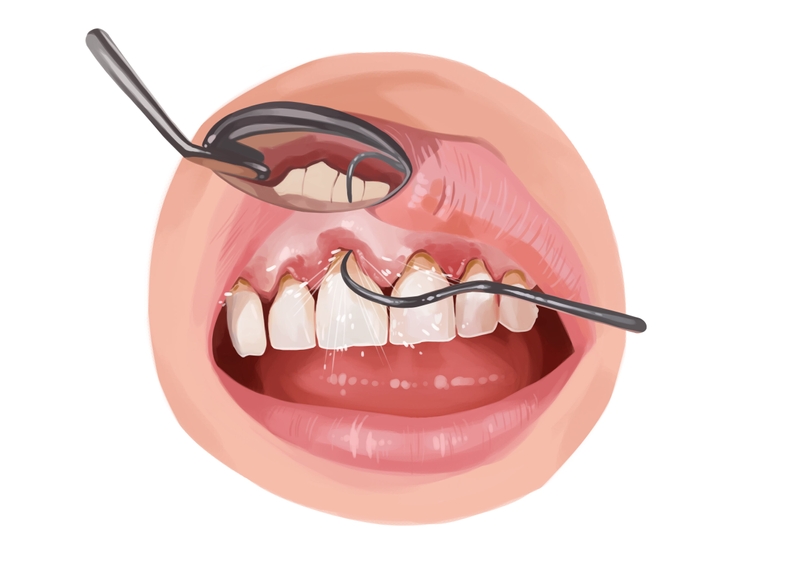
Picture by Authority Dental under CC 2.0 license
Decay on the teeth happens when bacteria multiply. Their by-product is an acid that breaks down tooth structure. With root cavities, this takes place at the level of the cementum. It is much softer than enamel and much more vulnerable to these acids.
Root caries develop twice as fast as regular cavities. This is even quicker when roots are exposed, for example due to gum recession or periodontal disease. The condition is quite common, with 9 out of 10 Americans having some untreated tooth or root decay.
Root decay symptoms
Some patients might not experience any symptoms. The diagnosis can then happen through a careful exam by a dental professional or on X-rays. Others might notice:
toothache that doesn’t go away with medication,
difficulty in chewing,
sensitivity to hot and cold temperatures,
discoloration of the teeth,
redness, pus, and swelling on the gums, as well as
loose, broken, or cracked teeth.
If you experience any of these, report to your dentist.
What causes root cavities?
The number one cause of root decay is poor oral hygiene. Patients who don’t brush and floss properly are at a high risk. Nonetheless, root caries are usually an effect of a combination of factors, including:
habits like smoking, drinking alcohol frequently, and consuming a lot of sugar,
a diet rich in acidic fruit,
aggressive brushing,
periodontal disease,
genetics,
diabetes,
stomach-related GERD,
age,
overcrowded and crooked teeth,
certain medications, and
trauma.
Aggressive brushing and gum recession tend to coincide. This is because vigorous action of soft tissues can make them sensitive and prone to infection. This in turn, can lead to gum disease.
Root decay treatment
Picture by Authority Dental under CC 2.0 license
If a root cavity is caught early on, the dentist may be able to reverse the process without much invasive treatment. This is why regular dental exams are so important. It can save you not only stress, but a lot of money as well.
Your dentist performs a visual exam and takes radiographs. This allows him or her to see what is happening on the surface as well as inside the soft and hard tissues. Gum recession is usually an indicator of more severe problems, however it does make root caries easier to identify.
Mild cases
If the decay is not severe, you may get away with less drastic measures. These include tooth remineralization and a professional teeth cleaning.
Remineralization is usually completed with fluoride treatments. You may be advised to use fluoridated prescription toothpaste and mouthwash. The dentist might also provide you with trays that you insert into your mouth every day for a short period of time. To remineralize your teeth avoid eating, drinking, or brushing your teeth for 30 minutes after application.
A professional teeth cleaning removes plaque, calculus, and tartar that you wouldn’t be able to get rid of yourself. Special equipment is used to get rid of these substances from the surfaces of the teeth as well as between them. Such treatment is recommended at least once a year anyway.
Severe cases
There are a few ways the dentist can try to save a tooth that has a decaying root.
The first course of action is to remove the damaged area and fill the hole with restorative material. This is similar to a filling, with either composite resin or amalgam.
If the root cause was gum disease, periodontal therapy is performed. Scaling and root planing with a combination of time-release antibiotics is the way to go.
The last resort before extracting the tooth is root canal treatment. These cavities are closer to the pulp than ones that appear on the surface of enamel. In the case that the pulp has become infected, the dentist or endodontist will open up the tooth to clean out the canals.
Sometimes this is still not enough. A badly damaged tooth has to be extracted to prevent the rest of the mouth from becoming infected. After removing the tooth, most dentists recommend replacing the space with fixed bridge or implant restoration. Implant restorations prevent bone loss and other complications to do with edentulism.
The most durable solutions are dental crowns (if the tooth has survived) or implants (if the tooth was extracted).
How to prevent root caries
The following tips can help you avoid root caries and complications they come with.
Brush and floss your teeth at least twice a day.
Use fluoride toothpaste and mouthwash.
If you have trouble with manual dexterity, invest in an electric toothbrush with a pressure sensor.
Do not smoke or drink alcohol excessively.
Control the amount of sugar, acidic fruits, and carbohydrates in your diet.
Visit your dentist for regular dental exams and cleanings.
Ask him or her about in-office fluoride treatments.
Report any gum recession or pain in your mouth.
FAQ
FAQ
Can root decay be fixed?
Are root cavities painful?