- Dental implants can be a successful tooth restoration option for diabetics if the diabetes is under metabolic control. It is a crucial factor in determining the success of dental implants.
- Diabetics are not good candidates for one-day implants. The longer a person has suffered from diabetes, the greater the chances of implant failure.
- Type 1 diabetics are more at risk of implant failure than type 2 diabetics.
Discover your smile's true potential. Use Authority Dental to book a dentist who does dental implants in your town. It's simple, fast and reliable.
Are dental implants safe for diabetics? Here's everything you need to know.
1. Dental implant survival in well-controlled diabetic patients is comparable to that of the general population
Picture by Authority Dental under CC 2.0 license
Harry Lee, DMD, explains: "The question of whether a person with diabetes can get dental implants is extremely common in my office, and the simple answer is a resounding yes, with a major asterisk. From my experience and the consensus among periodontists, well-controlled diabetes is not a contraindication for a successful implant."
"The true deciding factor isn't the diagnosis itself, but the patient's metabolic control, which we often assess using the A1C test," he emphasizes.
If diabetes is under metabolic control, it is not a contraindication to dental implants. The success rate is similar to that of non-diabetics, about 96.4%-100%. This concerns both type I and type II diabetes.
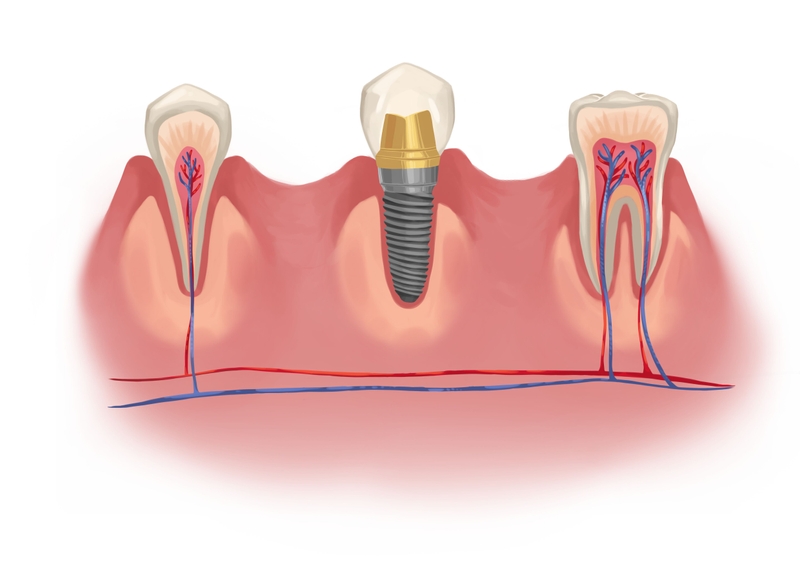
There are two key differences between healthy and diabetic patients getting implants. Firstly, diabetics must go through an antibiotic course. Secondly, the process of osseointegration is faster in healthy patients during the initial period.
2. Metabolic control is a key factor determining the success of dental implants
High sugar levels in the blood can affect the nerves negatively. This leads to constriction of blood vessels and poor circulation. That’s why healing in general is slower in patients affected by diabetes. The problem is magnified when the disorder is not controlled. Tests such as A1C will help determine control.

Dental implants involve not only the initial surgery but also a lot of regeneration. There are side effects when the body is not able to do this effectively. Implants can become loose, get infected, or even fail. When metabolic control is achieved, these are minimal.
3. Diabetics are not good candidates for one-day implants
Fast healing is vital when it comes to same-day implants. Since diabetes makes recovery slower, immediate load or mini implants are not the best choice.
Dentists recommend traditional implant placement for diabetics. This includes months of healing between stages. You are likely going to have to wear temporary crowns or go without any restoration for a while.
For diabetics who need full mouth restoration, dentists suggest the All-on-4 option. The design allows patients with less bone in the jaw to get implants. The rods are placed at an angle, and less pressure lies on the ridge.
4. The longer you’ve been suffering from diabetes, the bigger the chance of implant failure

Picture by Authority Dental under CC 2.0 license
Longer suffering from diabetes slows healing more. This disorder also makes you more prone to infections in the long term. Implants require a clean environment to heal properly. Any contamination could hurt the chance of survival.
Diabetics who are interested in getting dental implants should begin the process as soon as possible. The younger you are, the higher the chance of success.

5. Those with type I diabetes are more at risk of a failed implant
Diabetes must be well-controlled in order for a patient to be a good candidate for implants. Because of the faster rate of insulin consumption, type 1 is more difficult to manage than type 2.
This means type I is associated with a higher rate of failure. It is not impossible for such patients to restore their teeth with implants, but it requires more consistent work.
6. Early failure is a little more probable than late failure in diabetic patients
Early failure happens in the first days following dental implant surgery, before osseointegration.

The long-term success rate of dental implants is similar in diabetic and non-diabetic patients. Late failure is usually caused by patient-oriented risk factors such as smoking and poor oral hygiene.
7. The survival of implants in diabetic individuals can be improved by proper pre- and post-implant care
The process of getting implants as a diabetic may be a bit different. Changes in the diet pre- and post-operation, as well as special medicine courses, might be necessary.
Prophylactic antibiotics are usually not advised, but they can be beneficial in diabetic patients. The implants are also sometimes coated with bioactive material, have a different height and width, and chlorhexidine mouthwash might be required.
8. Dental implants are a better tooth restoration option than dentures for diabetics

Picture by Authority Dental under CC 2.0 license
Implants are a solution to inflammation, irritation, and infections that come with dentures. If you are a diabetic with missing teeth, this might be a better solution for you.
The disorder can make these conditions worse by making healing slower and complications more likely. Dental implants, due to their design, eliminate these problems. They sit firmly in the bone and come to no more contact with the gums than natural teeth do.
9. Peri-implant inflammation seems to be more common in diabetic patients in the long term
HbA1c values must be under control during and after the process of getting implants. Increased amounts often come with inflammation around the rod. This trend is especially visible after about 2 years.
Peri-implant inflammation can lead to a serious dental emergency and eventually to loss of an implant. It is very bad for your body to have inflammation anywhere for long periods of time. If you don’t control your HbA1c values, your dentist might opt to remove the implant.
10. It’s hard to conclude that uncontrolled diabetes leads to a higher dental implant failure rate
Most studies on the topic conclude that there is not enough hard evidence to suggest that diabetes brings a higher failure rate of implants. It would be unethical to conduct an experiment that would keep a test group in poor glycemic control on purpose.
Overall, diabetics with implants are usually motivated to keep their HbA1c values down, especially after the placement procedure. As long as you have a trusted specialist and disclose all of your conditions and medical history, diabetes does not have to be a contraindication.

FAQ
Are implants a good solution for both type I and II diabetes?
When diabetes is under metabolic control, the success rate is similar to that of those unaffected by the disorder. This goes for both type I and type II diabetes.
Nonetheless, type I may turn out to be more difficult to control. You need to work on it consistently to avoid failure. Statistics show that type 1 diabetes is linked to more implant failures.
How does diabetes affect dental treatment?
Poorly-controlled diabetes is linked to a higher chance of dental problems. Those patients may require more visits to the dentist in order to maintain good oral health.
The issues that affect diabetics more include infections, tooth loss, dry mouth, and gum disease. This is because their bodies have a harder time fighting off viruses and bacteria. What’s more, high blood sugar levels can lead to a faster development of those infections.
What can you do to increase the chance of dental implant success if you are a diabetic?
The most important thing is to get your diabetes under control. When blood sugar levels are steady, diabetes-related risks are minimized.
It is always key to maintain excellent oral health during the implant process, but it’s even more important when the patient is a diabetic. At all costs, avoid infection. It will be harder for you to fight it off than for regular folk.
Consider getting implants as soon as possible. The longer you have been suffering, the higher the chance of implant loss. Your dentist may also prescribe preventive antibiotics to increase your odds.
References
- Dental implants and diabetes mellitus—a systematic review
- Diabetes and Its Effect on Bone and Fracture Healing
- A Critical Review of Diabetes, Glycemic Control and Dental Implant Therapy
- Dental Implant Placement in Type II Diabetics: A Review of the Literature
- Oral Manifestations and Complications of Diabetes Mellitus
- Dental implant survival in diabetic patients; Review and recommendations
Nichole McKenna, DDS
Antibiotics prior to implant surgery is becoming quite common for all patients.